Meet ConfigureNet™, our large and rapidly expanding nationwide provider network enabling customers to have access to a full range of out-of-network physicians, specialists, hospitals, and healthcare facilities at a competitive price. Out-of-network claims savings are activated by ConfigureNet™ Price Advantage, our powerful cost-containment solution designed to protect people from the often unpredictable nature of out-of-network claims utilization. The ConfigureNet™ provider network also includes the Devon Health™ network, offering access to providers across PA, DE, NJ, and NY.
We’d love to help you leverage the power of our network to:
- Help control costs.
- Achieve savings for payors and health plan members.
- Contribute to enhanced member satisfaction for recruitment and retention.
Discover the flexible claims repricing solution that’s all upside.
Now you can leverage the strength of our ConfigureNet™ provider network’s market-leading, pre-negotiated rates with ConfigureNet™ Price Advantage. It’s a cost-containment offering that provides a no-hassle way to positively impact your employee- or provider-sponsored health plan’s bottom line and your plan members’ out-of-pocket costs when they access out-of-network care.
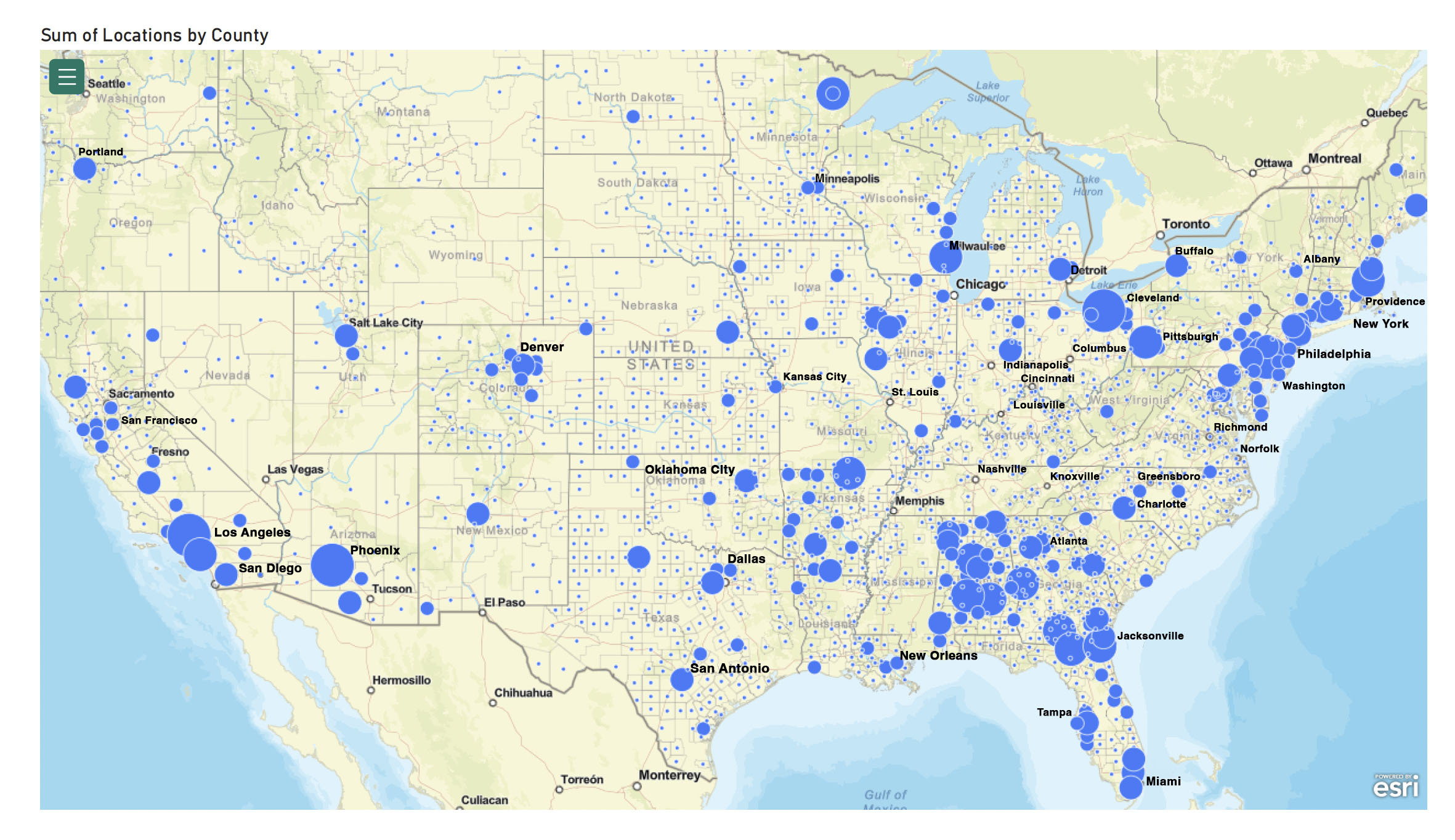
Access a national network of providers.
U.S. provider locations in all 50 states—coast to coast and everywhere in between.
The ConfigureNet™ provider network will bring nationwide access to providers with pre-negotiated contracts in place, including:
- Acute Care Hospitals
- Ancillary Facilities
- Chiropractors
- Durable Medical Equipment Suppliers
- Home Health Services
- Laboratories
- Mental Health Practitioners
- MRI Centers
- Physical Therapists
- Physicians
- Radiology Centers
- Surgery Centers
- Urgent Care Clinics
- … and more coming
The right solutions when you need them.
Through innovative products and services, we’re working to address the distinct needs of employer- and provider-sponsored health plans that provide health insurance for nearly half of all Americans.
Our ConfigureNet™ provider directory is a gateway to providers from coast to coast for your out-of-network health plan coverage needs. Access a directory of our providers.


We’re backed by the strength of Premier, Inc.
Premier, Inc., is on a mission to improve the health of communities. Premier is a leading performance improvement company serving more than 4,350 hospitals and health systems and approximately 300,000 other providers and organizations. As a consolidated subsidiary of Premier, Contigo Health, LLC is driven to create positive healthcare change and help provide access to cost-effective and high-quality care for all.