The Payvider Movement
Part 3 of 3: How to make your payvider solution a reality
Read Part 1: What Is a Payvider, and Why Should Health Systems Make Their Strategic Move Now?
Read Part 2: What is the Business Impetus to Become a Payvider?
In Parts 1 and 2 of The Payvider Movement series, we laid out the challenges health system leaders are facing in today’s healthcare climate, primarily feeling pressure to achieve greater financial and strategic impact in their organizations in an environment that is making that more difficult than ever. Many have looked at the payvider (payor and provider) model as a potential solution to satisfy their growth goals, since becoming a payvider has potential to drive new revenue, create valuable new relationships with large employers, and help health systems secure greater control of care delivery—all while empowering them to actively contribute to healthcare reform. Today, as market factors and technology are favoring the payvider model, the time to act appears to be prime. But how does a health system—perhaps your own—pursue the payvider path for its organization?
Moving from concept to a concrete offering
If you are a health system leader, you may be convinced that the payvider model is a good idea whose time has come for your system. But now what? You want it to work, but how can you get it started, and what all is it going to take to make it a reality, especially on top of your day job? In this final installment of our payvider series, we will look at the practical aspects of establishing a payvider solution, including how to leverage assets that may already be in place, determining what additional components will need to be created, and tapping into the expertise of resources that can be invaluable in helping to get the job done and done right.
The good news? You’ve already got a lot going for you.
The place to start when launching a new health plan offering is to leverage current strengths to the health system’s advantage and to ensure that the right expertise and partners are engaged to help avoid common pitfalls. Fortunately, most health systems already have a substantial number of elements already working for them. Virtually all health systems have existing strengths that make them well positioned to give employers and their health plan members the “Triple Aim” of cost, quality, and experience. In thinking about their own organization, they should consider the value of the trust and goodwill that have been established by the health system over the course of years within their local community. Chances are they have earned strong market recognition and brand loyalty that can be leveraged in a payvider solution. Additionally, every health system has clinical areas where it excels and where it can truly be said to offer the highest-quality care in the region. Whether it’s a robust and successful primary care model, cutting-edge clinical trials, or world-renowned surgeons, knowing your strengths is a key component to success. Leaders are encouraged to take a fresh look at their organizations and consider the value that they may currently take for granted.
In addition to your traditional care delivery, what additional programs and services does your system offer that can help set you apart? Does your health system have proven care coordination and navigation capabilities? Sophisticated care management programs? Is your system an established accountable care organization (ACO)? Perhaps your organization has a team-based, longitudinal care approach, or provides integrated care navigation and case and/or disease management through a patient-centered medical home (PCMH) model. Population health or bundled payment programs, such as surgery or chronic care, can give a health system a good head start on the payvider solution. Is there clinical data interoperability with the integrated delivery system? The first step in the payvider process is to assess every aspect of the care, approaches, models, and systems that are already in place within the health system and to recognize their value, along with the immeasurable power of the organization’s reputation, in setting the stage for a successful payvider solution. Building upon the existing and proven strengths of the health system, leaders must then develop several distinct components to support the new payvider model.
The “Functional Five”
In order for a health system to create the essential high-functioning integrated delivery and finance systems it will need as a successful payvider, the following five functional actions are essential:
1. Optimize care delivery systems
2. Get comfortable with data
3. Become as good at care payment as you are at care delivery
4. Establish valuable network operations
5. Become proficient in business development and working with employers
For the sake of clarity, let’s examine each in more detail.
Optimize care delivery systems
Health systems embarking on the payvider journey will find it beneficial to go all in on “systemness”—in other words, committing to integration. An example of systemness is the sharing of data and patient information; shared best practices and clinical pathways; team-based care, including both primary care physicians and supporting providers such as nurse practitioners; integration of behavioral health and medical care; and better assimilation of primary care and specialty care.
“Foundational to payvider success is creating a clear, tangible differentiator and delivering on that value through an integrated ecosystem.”
—Marisa Boevers, Vice President of Product Development and Management, Contigo Health
As Robert Pearl wrote in reference to the recent Kaiser acquisition of Geisinger and the formation of Risant Health, Geisinger will need to incorporate the fee-for-service community providers that it relies upon today more formally into the delivery system if it is to be successful.1 In his words, “To meet the healthcare needs of most its patients, Geisinger relies on community doctors who are paid on a fee-for-service basis. Generally, the fee-for-service model is predicated on the assumption that higher quality and greater convenience require higher prices and increased costs. With Geisinger’s distributed model, it’ll be very difficult to deliver consistent, value-based care.”
Get comfortable with data
As noted in Parts 1 and 2 of The Payvider Movement series, data and analytics, along with market dynamics, have evolved in the favor of health systems waiting to launch their payvider strategy. Economics and healthcare market forces established the need for innovations such as the payvider solution, and now, advanced data and analytics have made the payvider model viable. But that also means health systems must both embrace data and become proficient at using it to its fullest potential. It is vital to recognize data’s central role in order to knowledgeably and successfully optimize and scale the health plan.
The 2021 HFMA Health Risk-Based Healthcare Market Trend report identified “data integrity, reporting, and the cost of technology” as the leading internal challenges for health systems pursuing increased levels of risk.2 In fact, data was named more often than collaboration, scale, and difficulty achieving quality/cost outcomes. That HFMA survey also highlights several specific mission-critical roles data plays for the health system as payvider. For instance, bringing together clinical and claims data sources effectively delivers the highest value for both sides of cost and care. That stated, it also requires significant investment in both sophisticated technology and expertise. From the perspectives of clinical care, cost efficiency, and consumer experience, establishing the appropriate types and combination of benchmarking, analytics, reporting, and clinical technologies is vital to making smart, collaborative payor-provider decisions. Additionally, having quantifiable intelligence that reaches beyond your health system and health plan members provides rigor when establishing strategies that bridge cost, quality, and operational areas of the provider-sponsored health plan. Only at this level of data analysis are leaders able to align provider incentives that facilitate further investment in preventive care and quality management. Securing actionable intelligence that can improve outcomes, support enhanced financial performance, and enable success in new, alternative payment models is what will make managing an integrated risk-based approach possible.
Become as good at care payment as you are at care delivery
Getting the care delivery and data side right is certainly fundamental to the success of any payvider model. Establishing efficient health plan operations is critical as well.
This includes:
• Eligibility and enrollment operations
• Claims adjudication and appeals
• Auditing and compliance processes and reporting
The payvider will also need to decide if they want to recreate some of the traditional care management functions common to payors, such as case management, disease management, and utilization management. Depending on the plan design, payment method, and “systemness,” health systems functioning as payviders may be able to eliminate most or all these oversight functions by incorporating tools such as clinical decision support, clinical pathways, and risk transfer to ensure the care being delivered meets the goal of the Triple Aim (cost, quality, and experience). Health systems would also be well served to take a good, hard look at their cost structures and determine what shifts may be necessary. For instance, health system payviders may want to offer a combination of fee-for-service and value-based care, especially in early years. The health system as payvider can be the powerful and much-needed catalyst for payment reform. Capitation is an excellent way for health system payviders to capture the value they create in “value-based care.” Capitation allows health systems to evolve their facilities and staffing models beyond a focus on the services delivering the highest reimbursement and on to those services that best meet the needs of their community.
Regardless of the preferred payment methodology, to be a successful payvider, health systems must be able to manage the cost trend. Effective ways to accomplish this include eliminating low-quality and inappropriate care, using digital enablement and team-based approaches to make care delivery more efficient, promoting early intervention with health plan members to improve outcomes, and establishing a true cost-based accounting system to understand more accurately what the “cost of goods sold” is and, from there, know how to set fair and transparent prices for each. Even with the aid of these tools, payviders will still need to have effective ways to communicate and connect with members. Such communication can be enabled by digital support systems that are designed to help providers give health plan members the little nudges they need to adopt healthy behavior—whether that be medication compliance, lifestyle choices, or helping them determine whether to pursue conservative treatment versus surgery.
Establish valuable network operations
One of the cornerstone elements of success as a payvider is the forming of or joining in a narrow network. The narrow network is advantageous in that it can drive appropriate volume in the early years for the payvider while the health system is primarily employing fee-for-service arrangements. The narrow network also enables the health system to filter out any high-cost, low-quality providers from the mix. This becomes particularly important as the payvider introduces attractive capitated or value-based care arrangements. Beyond the network, the health system must establish transparency and execute suitable contracts with its own employed physicians. It can also be tremendously valuable to have a relationship with a network resource such as Contigo Health, LLC that understands health system payviders intimately and has the expertise and reach to help introduce additional regional and national providers to the health system that meet established value standards.
Become proficient in business development and working with employers
Understanding how employer health plans work and what employers want most is the leaping-off point. To meaningfully approach and engage prospective employers, one must know what pains they are experiencing and what is needed most from their health plan for both members and their business. Such understanding can begin with introspection into your own health system’s experience as a sizable employer in the community that operates its own self-funded health plan for employees. Beyond tapping into that firsthand knowledge, below are a few other things to consider.
Employers want care to be affordable.
Above all, employers are seeking affordability. After all, self-insured employers own the risk of their employees’ healthcare utilization. As such, they feel the direct impact of each swing and shift. These employers are acutely aware of how much care their employees receive and how much that care costs. That becomes particularly poignant considering that median costs per person increased to more than $6,000 in 2021, according to new analysis from the Health Care Cost Institute (HCCI).3 The study also indicates that median per-person healthcare spending increased by 24 percent from 2017 through 2021.4 Employers genuinely want value-based care to work. They want care that is affordable, high quality, and convenient (the Triple Aim).5
They know their employees aren’t as healthy as they should be.
Along with their concerns about rising costs of care, employers are also highly aware—and reasonably anxious—that their employees do not enjoy optimal health. Factors such as medical history, environmental factors, social determinants, lifestyle, and more are at play and are largely out of the employer’s control.
Unfortunately, the programs and benefits that employers invest in and put in place to mitigate these factors are commonly underutilized.6 With less-than-optimal employee health compounded by high costs of care, it is no wonder employers are placing stronger focus on employee well-being and benefits engagement. A 2023 Forrester Consulting study indicates that 80 percent of HR and EX professionals surveyed place increased emphasis on improving health benefits offerings, growing awareness of benefits, and making access easier.7 Even so, utilization remains low.8
They—and their employees—want convenience.
Employers and their health plan members want genuine convenience. They expect providers to have availability and to offer both in-person and virtual care options that make it easier for the member to access care.9 They also want access to the digital tools that make care management simpler, no matter where they are.10 While there may be structural challenges related to data and introducing new ways to make access to care more convenient, payviders may actually be in the ideal position to help remove much of the current confusion and inconvenience contributing to plan members feeling trapped between their care provider and their insurance carrier.
Beyond the employers themselves, it is essential to understand the brokers and consultants who work closely with employers as trusted advisors. It will be critical to know how to win their respect and trust so they won’t become a barrier between the health system and targeted local employers (and they can be a barrier if they are not engaged in the process early on). Instead of viewing the broker as an obstacle, health system leaders should consider the value brokers can bring as a source of precious insight into the targeted employer. If trust is established between the health system and broker—and the broker can see the value in what is being offered to their employer client—they can be an ally to the payvider. In fact, when approached properly, brokers and consultants can become the health system’s gateway to the employer and may even serve as an advocate and/or point person.
Once employer relationships are secured, it will be tremendously valuable to provide meaningful, timely reporting to all employer groups. One of the best ways to differentiate the health system payvider from traditional payors is to consistently and proactively deliver extensive, transparent reporting as well as access to data for those employers who prefer to do their own analytics. Remember that employer sales cycles are annual, but employers often begin their search for the next health plan carrier a full 18 to 24 months in advance of that plan going live. To put that in perspective for the health system just embarking on its payvider solution, it can take several years to form a health plan, have a pilot client (such as the health system’s own employee health plan), show the results, and develop a pipeline of prospects. Having a defined and disciplined approach to payvider development is crucial since slow decision-making, missed deadlines, or unclear objectives can result in lengthy delays and, most important, missing these long-term sales cycles and the opportunities they represent.
Going all in
Deciding to become a payvider is not a light decision. After all, it is a foundational change to a health system’s business that will impact everything it does. But it’s all for the better. Health-system-led payviders are positioned to drive true care transformation and improve the health and well-being of millions of Americans, drive toward a better healthcare ecosystem, and create much-needed financial stability and growth opportunities for themselves. But to get there, the health system must formally and firmly commit. Here are some of the ways to make that commitment pay off.
Hire a team.
You, the health plan leadership, need an experienced health plan/payvider leader to work with you, along with a dedicated team of specialists that includes:
• Health plan executive (leader)
• Legal, compliance, regulatory, and privacy
• Analytics
• Population health
• Business development
• Network/provider
Each of those areas needs to have at least one person on the health plan side dedicated to managing and overseeing vendors. This should not be someone from the health system attempting to do the job in addition to their regular job responsibilities; it is a full-time commitment and must be a dedicated resource without other obligations. While the requirements to establish the payvider model may feel overwhelming and the mountain of details may seem insurmountable, health system leaders need not go it alone. They can find it tremendously valuable to align with a knowledgeable strategic partner who is equally committed to realizing the health system’s payvider vision, to creating a sustainable healthcare ecosystem, and to putting providers back in the driver’s seat of care.
There is an organization dedicated to making it easier for health systems to activate a payvider solution and help connect health systems with employers. Born out of the healthcare industry as a consolidated subsidiary of Premier, Inc., Contigo Health has been down this road before, helping health systems initiate and grow their own payvider offering. Contigo Health is a health benefits platform that leads direct-to-employer and direct-to-provider relationships and is focused on revolutionizing healthcare through appropriate, cost-effective, transparent, and thoughtful benefits design—all in the interest of leading the way to financially sustainable healthcare. The Contigo Health® Payvider Activation product is designed specifically to guide and support health systems every step of the way.
In the end…is it all worth it?
Having a knowledgeable partner and a solution that is designed to provide a comprehensive approach and all the components needed certainly makes establishing a payvider solution more attractive and achievable. And knowing that the healthcare ecosystem status quo will not be a sustainable long-term solution for health systems wanting to be both viable and vibrant in the years to come is the impetus to make the move now while the market is favorable. Becoming a payvider is not a journey to be taken lightly, but it can be a tremendously rewarding one, especially when the effort is supported by knowledgeable payvider specialists who can help ensure everything is done properly.
Now what? Here’s a logical place to start.
To assist you in determining if becoming a payvider is right for your health system, Contigo Health is offering a complimentary payvider readiness assessment.*
The assessment will include:
• “Nine Facets of Payvider Readiness” internal self-assessment
• Market snapshot, including high-level evaluation of your addressable market, competitive landscape, and market dynamics
• Two-hour consultation with our payvider strategy team to review results and conduct a visual planning session
To learn more, please contact Marisa Boevers at marisa.boevers@contigohealth.com.
* Additional terms and conditions apply.
Sources:
1. Forbes. 2023. “Value-Based Healthcare Battle: Kaiser-Geisinger Vs. Amazon, CVS, Walmart.” July 2023. https://www.forbes.com/sites/robertpearl/2023/07/17/value-based-healthcare-battle-kaiser-geisinger-vs-amazon-cvs-walmart/?sh=38cabad16417. Accessed 11/03/2023.
2. Guidehouse. 2021. “2021-22 Risk-Based Healthcare Market Trends.” November 2021. https://guidehouse.com/-/media/www/site/insights/healthcare/2021/gated/2021-risk-based-healthcare-market-trends.ashx. Accessed 11/03/2023.
3. Health Care Cost Institute. 2023. “Healthy Marketplace Index.” June 2023. https://healthcostinstitute.org/hcci-originals/healthy-marketplace-index/hmi. Accessed 11/03/2023.
4. TechTarget/RevCycle Intelligence. 2023. “Median Per-Person Healthcare Spending Exceeds $6K.” July 2023. https://revcycleintelligence.com/news/median-per-person-healthcare-spending-exceeds-6k. Accessed 11/03/2023.
5. Health Affairs. 2008. “The Triple Aim: Care, Health, and Cost.” June 2008. https://www.healthaffairs.org/doi/10.1377/hlthaff.27.3.759
6. HLTH. 2023. “The Business Case for Boosting Benefits Engagement: Improving Employee Wellness, Retention, and the Bottom Line.” June 2023. https://www.hlth.com/digital-content/hlth-matters/blog/the-business-case-for-boosting-benefits-engagement-improving-employee-wellness-retention-and-the-bottom-line. Accessed 11/03/2023.
7. Ibid.
8. Ibid.
9. Kyruus Health. 2022. “Becker’s Payer Roundtable Recap: Are Payviders Supervillains or Superheroes?” November 2022. https://kyruushealth.com/beckers-payer-roundtable-recap/. Accessed 11/03/2023.
10. Ibid.
© 2024. Contigo Health, LLC. All rights reserved.
The Payvider Movement
Part 2 of 3: What is the business impetus to become a payvider?
Read Part 1: What Is a Payvider, and Why Should Health Systems Make Their Strategic Move Now?
Read Part 3: How to Make Your Payvider Solution a Reality
A concept whose time has arrived.
Health system leaders are feeling increasing pressure to achieve greater financial and strategic impact for their organizations. At the same time, the current healthcare environment is making it more challenging for them to do so. In their efforts to find viable solutions, many health systems are now weighing the pros and cons of creating their own payvider solution, taking on the roles of both payor and provider. As covered in Part One of this three-part series, the timing for the payvider strategy appears to be right for those health systems seeking to secure greater control of both financial and clinical realms of healthcare and interested in pursuing new avenues of growth. But, while market forces are making this move feel intuitively right, it is important to take a hard look at whether this is the right move for your organization, both strategically and financially. In this installment, we will present the business case for establishing a payvider solution.
What the payvider model can do for today’s health systems
Becoming a payvider offers financial value, such as driving additional revenue for the health system, as well as strategic value. That can include building the health system’s brand and position, developing relationships with regional employers and individuals, and providing greater control in negotiations with other payors. Perhaps most important, it can give health systems the opportunity to lead in healthcare reform by providing them with a mechanism to align incentives and deliver high-quality care at a fair price.
The Hard Facts: Tangible Values of Becoming a Payvider
Market share growth
An increasingly attractive way for health systems to establish growth is to introduce a payvider solution that can enable them to capture a greater portion of their market by engaging area employers. The payvider model can ensure a steady stream of patients, with fair reimbursement rates that are paid by those patients’ employers. Establishing prepaid (also known as capitated) plans or services can further help to drive steady and predictable revenue. For even greater growth, the most successful payviders participate within narrow networks that can efficiently drive patient care volume to high-quality providers while eliminating low-value providers that tend to be high-cost and/or low-quality options. In addition to driving growth for the health system, it can be both clinically and financially beneficial for patients.
Revenue diversification
Although health plan profits likely won’t outpace the delivery-side revenue, the payvider model can create a steady revenue stream opportunity that is separate from the health system’s traditional care-delivery income. Those diverse revenue streams can be generated by a combination of administrative fees, wellness and disease management programs, pharmacy, stop-loss insurance, voluntary benefits, and more.
Value-based care success
Although many systems have had success in value-based care arrangements, partial or full capitation, and other risk-based arrangements without becoming a payvider, becoming a payvider and offering products like this directly to employers without another intermediary can be financially rewarding for health systems. Using all the levers of population, including plan design and member incentives and engagement, coupled with the health system’s resources, providers who become payviders are in the enviable position to make at-risk payment arrangements profitable.
The Softer Side: The Nonfinancial Value of Becoming a Payvider
Be a catalyst for change
While medicine continues to make great advancements in the twenty-first century, healthcare providers largely remain stuck in an outdated twentieth-century health system construct. Most health systems continue to carry the burden of enormous overhead and human resource fixed costs. Meanwhile, population health needs are becoming increasingly less episodic and more longitudinal, setting the stage for long-term management of chronic conditions (e.g., metabolic disease, behavioral health, and subacute conditions such as autoimmune diseases and some cancers). However, the archaic health system construct is simply not set up to deliver the care needed in today’s rapidly evolving landscape. Here are just three examples of how the construct is mismatched to today’s needs, capabilities, and market demands:
- Health systems are heavy on facilities, but a significant portion of care can now be delivered effectively as outpatient or in-home.
- Care delivery models are overly physician-centric and would benefit by evolving to leverage other qualified providers, including nurse practitioners and pharmacists, to deliver care where appropriate.
- Current practices do not take advantage of available technology and remain too focused on the in-person visit rather than taking advantage of asynchronous communication and automation of repetitive tasks.
For a payvider, the incentives are all aligned for health system leaders to drive real change—not just payment reform, but also care transformation. By consolidating both delivery and finance under one strategic leadership team, payviders create opportunities to reconstruct the system and make progress toward the Quadruple Aim.
Build the brand and defend the strategic position
Becoming a payvider can enable a health system to regain control and create a strategic moat around themselves that can help prevent other payors or disrupters, such as independent direct primary care or virtual care companies, from significantly impacting their markets. The payvider model can also create a desirable “sticky” ecosystem that encourages high loyalty from both patients and referring physicians, leading to sustained revenue streams and growth. Because the payvider model puts the provider in the driver’s seat, health systems are better able to drive care transformation, enabling them to do the right thing for the patient while simultaneously contributing to much-needed payment reform. It’s what some might call a win-win scenario.
Exploring the Business Case for Payvider
In today’s healthcare climate, there appears to be no shortage of factors that make the payvider solution attractive and worth pursuing. But is it a good financial decision? One of the most important factors for any health system considering the move is the business case for becoming a payvider. While it is not practical in this format to present the specific financial picture for every size and type of health system in every U.S. market (although individual scenarios can be provided by Contigo Health, LLC upon request), it is possible to illustrate the business case by using a midsized health system model and reliable national health plan membership data to represent a typical scenario. First things first: let’s begin by creating the framework.
Establishing a baseline
What might the numbers look like for an average health system? Let us begin by establishing a workable baseline. Considering national averages,1 we can approximate the numbers for health plan membership in the United States:
- Administrative and network access costs are approximately $40 per member per month (PMPM)
- Wellness and disease management programs beyond core health plan fees (a.k.a. buy-ups) are about $4 PMPM
- Care-delivery fees average about $5,904 per member per year (PMPY)*
*The above is based on a report from the Kaiser Family Foundation indicating that the average employee total annual premium for health insurance in the U.S. is $7,380.2 Since administrative costs and profits account for about 20 percent of that premium, the amortized care costs per health plan member per year would be $5,904.
For our hypothetical example, we will apply those figures to a midsized health system in a top-25 midwestern city having 2,000 beds and 18,000 employees.
Projecting revenue
With a baseline set, we can examine the business case for the payvider solution over a five-year span that begins with the health system’s own health plan in the first year and then expands to area employers and beyond in subsequent years.
Year One: Payvider for the Health System
In the first year of implementation, Contigo Health recommends that the health system create its payvider model for its own employees. This enables the health system to build, learn, and refine its payvider offering within its own enterprise while creating a case study that can be leveraged later when promoting their payvider solution to other employers. Here is how the payvider model could benefit the health system, even when limiting the solution to its own employees. Assuming a health plan covering 40,000 lives, composed of health system employees and their dependents, and a total benefit budget of approximately $295 million, the following can be surmised: Savings can be achieved through flexibility and smart design. If the payvider’s employee benefit plan is a traditional ASO (administrative services only) contract with a large national carrier, then in switching to their own plan administered by a neutral third party, they can experience savings driven by increasing domestic utilization, creating direct contracts with high-utilization nondomestic providers, and using their own care management and care navigation capabilities to ensure their employees access only high-quality, appropriate care.
Our example health system payvider, through smart benefit design and improved provider selection programs managed by the health system, successfully increases domestic utilization from 70 percent to 80 percent, resulting in $29.5 million in cost savings. They save another 5 percent, or about $15 million, by creating direct contracts with a local children’s hospital and oncology centers. Finally, our example health system payvider holds their total utilization flat, primarily by increasing access and incentivizing their employees to use their advanced primary care teams. Those teams effectively manage chronic disease and reduce inappropriate care, enabling the system to counter the projected 7 percent increase across the industry. Even if the health system maintains a flat trend, the health plan’s projected savings would still be $20.65 million.
In Year One, by applying its payvider solution only to its own employees, the average midsized health system could expect to see a combination of savings and cost avoidance totaling close to $65 million.
Year Two: Payvider for the Market
Equipped to leverage its experience as a payvider to its own health system employees, the health system is prepared to go to market with a payvider health plan whose benefit design features capitated (prepaid) primary care plus fee-for-service specialty care using a point-of-service plan design. For the sake of this business case, we will assume that the health system has successfully enrolled the following employers in its payvider solution:
17,600 lives
One large group of city employees representing a total of 17,600 lives (8,000 employees plus dependents)
1,540 lives
Five small area employers representing a total of 1,540 lives (700 employees plus dependents)
1,200 lives
A portion of a national employer with a significant workforce in the region, representing 1,200 enrolled lives
In this reasonable Year Two expansion scenario, the health system adds 20,340 lives beyond those already within its own employee plan. Those additional nonemployee lives generate $9,763,200 in core health plan administration fees, delivering a 5 percent margin of $488,160. They also generate $976,320 in disease management program fees, producing a 10 percent profit of $97,632. The prepaid primary care, billed at $400 per member per year, generates $8,136,000 in care delivery. All care that falls outside of the scope of primary care is estimated at $4,500 per life annually, adding up to $91,530,000. Assuming that 80 percent of that care is to be delivered domestically (after all, the payvider influences domestic utilization), that equates to $73,224,000. If the health system historically claimed 50 percent of the market, it can be assumed that 50 percent of that care, or $36,612,000, is net new revenue for the health system.
Year Two adds:
20,340
non–health system employee lives
$97,632
in disease management program fee profit (10 percent of $976,320)
$488,160
in ASO fee margin (5 percent of $9,763,200 in ASO fees)
$8,136,000
in prepaid primary care ($400 PMPY)
$36,612,000
net new revenue (assuming provider market share of 50 percent)
$73,224,000
in nonprimary care (80 percent domestic utilization of $91,530,000)
Year Three: Payvider for the Region
Building on the success and momentum of Years One and Two, the health system can realistically continue to expand the growth of its payvider program’s nonemployee lives by 20 percent, reaching 24,408. Applying the same revenue line items presented in the Year Two example, the revenue opportunities become increasingly attractive in Year Three.
Profit on ASO fees at 5 percent now equals $263,606
Profit on disease management fees at 10 percent adds up to $117,158
Primary care capitation reaches $9,753,200
Domestic specialty care generates $87,868,800 equating to a net new revenue sum of $43,934,400
Years Four and Five: Payvider for All
With continued focus on growth, building on three years of successes, the payvider continues to establish 20 percent growth each year, resulting in new care revenue streams reaching $63,265,536.
Additional Growth via a National Narrow Network
In addition to the care revenue generated by the growing volume of lives covered by the health system’s payvider health plan, the payvider may want to consider participating in a national network composed of other payviders and health systems. As a member, the payvider can work together with others to win national account business, accelerate growth, and generate fees for members who live outside the current reach of the health plan’s service area. Conversely, the payvider can also generate additional care revenue at fair rates for those lives covered by other payviders within that narrow national network.
The Need—and the Numbers—Support Payvider
Provider acquisition by payors, the continuing shift to value-based care, and payor-provider partnerships that have failed to support the delivery systems can all create pressure on health systems. Rising costs and labor shortages compound the situation. Health system leaders seeking opportunity are looking more intently at the payvider solution. And, as has been laid out in this paper, the business case can be strong. Further, as covered in Part One of this series, technology, regulations, and market dynamics areindicating that now is the right time for health systems to make the move to become a payvider. The only remaining barrier for some is how to make it happen.
Contigo Health is a consolidated subsidiary of Premier, Inc. and is committed to leading the way to financially sustainable healthcare. As a health benefits platform that leads direct-to-employer and direct-to-provider relationships, Contigo Health is relentlessly focused on revolutionizing healthcare through appropriate, cost-effective, transparent, and thoughtful benefits design. One of those solutions is the Contigo Health® Payvider Activation program, which was developed to give health systems a comprehensive, turnkey payvider activation solution that presents everything needed to build and grow their own payvider program with confidence while minimizing risk.
Part Three of this three-part series will explore how health systems can operationalize a payvider solution and make it work while still managing their full-time responsibilities.
Sources:
1. Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Statistical Brief #543: Trends in Health Insurance at Private Employers, 2008-2021. July 2022. https://meps.ahrq.gov/data_files/publications/st543/stat543.shtml. Accessed 1/31/2024.
2. Ibid.
© 2024. Contigo Health, LLC. All rights reserved.
The Payvider Movement
Part 1 of 3: What is a payvider, and why should health systems make their strategic move now?
Read Part 2: What is the Business Impetus to Become a Payvider?
Read Part 3: How to Make Your Payvider Solution a Reality
Is this the age of the payvider?
By now, most health systems are familiar with the term “payvider” (an integrated delivery and finance system). Many have been weighing the pros and cons of initiating their own payvider solution, perhaps for years. But, for them, there has been no catalyst strong enough to set the payvider wheels in motion. That critical tipping point may well be here, however, as health systems feel increased pressure to make greater financial and strategic impact even as strong headwinds make it difficult to make the advances that will enable them to grow.
Fortunately, technology, regulations, and market dynamics have turned a corner and are now favoring those providers looking to become payviders. By all indications, the time to move on the payvider option is now.
Payvider 101 (What is a “payvider” anyway?)
A payvider is perhaps best described as an integrated delivery and finance system. In other words, it is an entity that sells and administers a health plan product and then delivers the associated care. It is both payor and provider (thus “payvider”).
The payvider solution works with a wide range of health plan structures, including self-insured groups, fully insured groups, individual and small groups, Medicare Fee-for-Service, Medicare Advantage, Medicaid, and more.
There are three payvider models:
1.
The joint venture model brings payors and providers together in alignment to develop their own health plans. Both share the same goals of improving patient care and attracting a greater number of members, although this model commonly puts the payor in the lead role.
2.
For the insurance company as provider model, the payor transitions to become the provider of healthcare. This gives the insurance company greater overall control of costs while adding some level of convenience for the member (since everything is handled by one entity).
3.
In a provider plan model, the health system creates its own health plan and retains control of the finances, having no obligation to share with other partners. The provider can put patient care at the forefront while fully benefiting from any and all savings they create through efficiency and quality improvements to their own healthcare services.
Model #3, the provider plan, puts the health system squarely in the driver’s seat, while models #1 and #2 take the provider out of that position of control. The joint venture and insurance company as provider models have rarely resulted in either financial stability for the health system or true care transformation.¹ Instead, they now represent the “corporatization of American healthcare,” a scenario in which providers are increasingly managed (versus managing) throughout the process and much of the value created is absorbed by the intermediaries versus being shared among providers, employers, and health plan members. The provider plan model is designed to mitigate those issues.
Why should a health system be motivated to become a payvider?
There are many reasons for a health system to become a payvider. First and foremost on many health systems’ minds are financial viability and stability. A payvider strategy can help health systems achieve that. Health systems that become payviders have the opportunity to build strong bonds with self-funded employer groups, thereby capturing market share and improving their payor mix. They can also add diversified revenue through administrative and program fees, as well as drive a significant cost savings on one of their organization’s largest expenses: their own employee health plan.
But the real motivation for becoming a payvider is the opportunity to drive care transformation through payment reforms and eliminating misaligned incentives and structural barriers, such as compensation design, that prevent many providers from delivering the best care in the most efficient manner.
Take for example the advanced primary care model, which uses a team-based, multimodal engagement approach to patient care. In this model, primary care physicians are able to have a larger patient panel while also spending more time with patients when needed by using a team of information-connected colleagues that includes nurse practitioners, clinical pharmacists, behavioral health providers, and care navigators to handle less-complex patients and routine tasks. This team-based medicine approach, enabled by real-time data sharing and secure member communication, lowers costs, improves outcomes and patient satisfaction, and reduces provider burnout. But most health plans don’t currently have strong reimbursement strategies for this optimal care delivery. When providers are integrated into the health plan, though, the payment redesign can help to drive the care redesign.
A provider-led payvider model (the provider plan) is perhaps the best way to achieve the true aim of value-based care: creating cost savings while simultaneously optimizing patient outcomes. Payviders also have access to better data and visibility. As Dr. Jonathan Slotkin, chief medical officer for Contigo Health, LLC observes, “Every successful provider-sponsored health plan that I have seen has had one key thing in common: each leverages modern data analytics and reporting technology to effectively manage both the provider and the payor sides of their health plan offering.”
The vital role of data and analytics
Economics and healthcare market forces stimulated the need for innovations such as payvider solutions, but it is advanced data and analytics that have made them viable. Bringing clinical and claims data together can:
- Deliver high value for both cost and care
- Help enhance financial performance while also improving outcomes
- Empower collaborative decisions around clinical care, cost efficiency,
and the consumer experience - Support new, alternative payment models
- Guide and motivate investment in preventive care and quality management²
With better access to data comes better management potential
The payvider that accesses data and analytics can establish a next-best-action (a.k.a. NBA) tool. This single integrated data repository captures a complete picture of a patient’s medical history, social determinants of health, current care plans, claims data, and more. Then, through algorithms and artificial intelligence, it helps identify the next best actions. The combined data also contributes to a more informed patient-centered medical home, providing plan members the necessary care coordination and navigation they need to help ensure the right care at the right time and place.
Such data can aid the primary care physician and full care team in guiding patients throughout their care journey. Further, benefit design and a network tiering structure can be optimized by data, helping to drive domestic utilization and promote use of in-network providers.
Additional advantages can include:
- Benefit and reimbursement strategy focused on advanced primary care, patient-centered medical home care, and preventive care
- High-value prior-authorization strategy, integrated communications, and situational rules, such as “gold carding”
- Integration of ancillary benefits, including pharmacy, dental, and vision, to support whole-person care
Better data leads to better management. And better management leads to better outcomes.
A recent survey³ of payors by Change Healthcare revealed that value-based care helps improve quality of care, patient engagement, and cost reduction:
Payors reported a 5.6% cost reduction related to unnecessary medical expenses.
80% reported increases in quality of medical care.
73% saw improved patient engagement.
Why NOW is the time to initiate a payvider solution
Health systems are feeling the need for change
Labor expense and shortages are now everyday trials. Capital markets are changing as bonds are downgraded. Traditional contracting is no longer working as payors increasingly squeeze providers. More than ever, health systems must make a positive impact, both financially and strategically. Unfortunately, many simply continue to rely on traditional approaches in this nontraditional environment, somehow expecting different results.
Cutting operating costs while discreetly raising prices, for instance, or adding ancillary services are merely short-term fixes. Instead, health systems needing healthy change must embrace a different strategy.
According to The Keckley Report,⁴ there are three distinct changes that providers must make now to find success in the future state of healthcare:
- Creating regional systems of health via cooperation among public health and health-delivery entities in the interest of sharing data and resources across multiple organizations
- Increasing competitive strength in price and value, made possible through the integration of financials and care delivery
- Emphasizing greater accountability by health plan members, fueled by infusing self-care in care management
The good news? The stars are aligning for the payvider solution
While health systems might have found it challenging to initiate their own payvider solution in the past, technology, regulation, and market dynamics have now shifted to health systems’ favor.
Today data integration is much improved thanks to more health information exchanges and fast healthcare interoperability resources data standards. There is greater information integration into electronic medical records, meaning that benefit design information, prior authorization, and preferred providers can now be integrated into clinical decision support systems. Meanwhile, the maturation of artificial intelligence and machine learning are accelerating next-best-actions tools, improving diagnostics, and enhancing population health trends.
On the regulation front, lawmakers are paying closer attention to healthcare affordability, access, and equity. New pricing-transparency requirements call attention to disparate rates between hospitals and payors and are driving normalization of market rates (all of which are addressed by the payvider solution).
At the same time, employers are growing increasingly frustrated as conventional approaches are no longer effective. Employers are now confronted with an aging employee population⁵ stricken with metabolic disease and chronic conditions including obesity, diabetes, and musculoskeletal issues.⁶ Younger employees are facing a higher incidence of cancer.⁷ Behavioral health and substance use disorder issues have exploded since the pandemic.⁸
Employers are ready for a better solution. Beyond the factors making it practical to initiate a payvider solution, there are also emerging opportunities for health systems who do so. With more providers entering the value-based care space come new occasions to create mutually beneficial arrangements. For instance, syndicate networks bring regional health systems together to enable access to high-quality, high-value care outside of a single hospital service area. Health systems also have the opportunity to create a payvider network, with each participating health system offering reciprocal care and rates in the interest of serving employer groups having multiple locations, remote workers, or travelers that extend the call for care beyond the local service area.
By creating a national primary network, payviders can eliminate dependence on specialty wrap networks.
With good news comes greater risk to those who wait
Perhaps the greatest incentive to act now is that others are already making the move.
More providers are experiencing a sense of urgency as industry disruption forces them to rethink current payor and provider partnerships and reassess where their best opportunities lie moving forward. Payors don’t want to miss out either and are vigorously building and investing in primary care resources so they can capture control of where and how care is delivered.
As the carriers dive deeper into this space, and as value-based care comes to the commercial/employer plans, if health systems fail to create their own payvider solutions now, they risk being consumed by the carrier’s solutions. Without the strength of their own payvider program, providers stand to lose valuable leverage in network negotiations and could see their market share eroded by third-party disrupters offering point solutions and alternative care-delivery options. Conversely, a payvider strategy helps health systems create a barrier of protection—a strategic moat of sorts—against payors and other market disrupters.
Simply put, health systems must evolve to survive. Fortunately, that has become more viable and attractive than ever.
Evidence that payvider works
More than 300 U.S. health systems currently have some sort of health plan.⁹ Having a unique ability to see and navigate the entire care experience (after all, they are providing the care), the payvider then has the added benefit of greater visibility and increased influence. Here are a few real-world examples of payvider solutions.
Kaiser Permanente, as of June 30, 2023, has a health plan with 12.7 million members (up 81,000 members since December 31, 2022),10 an annual operating revenue of $95.4 billion in 2022,11 and a high market share, including the highest rankings in six key regions.12 According to Forbes, in 2023 the plan earned an average grade of 4.3 out of 5 from the National Committee for Quality Assurance.13 Kaiser Permanente continues to earn a strong reputation for its blend of low cost and high quality,14 thanks to the integration of health plan and care systems and its focus on prepaid (capitated) products, including HMOs and EPOs.
UW Health/Quartz exemplifies how the payvider solution can contribute to financial strength for a health system, as illustrated in a recent article by the Foundation of the American College of Healthcare Executives (FACHE). Creating its own health plan allowed UW to mitigate swings in the market and recover from the unexpected volume changes and loss of high-margin elective procedures caused by the COVID-19 pandemic.15 Also, predictable capitation payments enabled UW to diversify revenue and achieve financial stability, ending each year with positive margins while other systems in the fee-for-service world saw financial devastation. Further, because UW owns its own plan, it has been able to invest in care innovations, like virtual care and other digital capabilities—including a hospital-at-home care model—all fully or partially funded by the savings afforded by its plan’s capitated population.
Phoenix-based Banner Health and CVS Health business Aetna came together to form a joint-venture health plan in 2016 in their pursuit of a value-based care model.16 Based on the success of that venture—citing an average cost savings of 8%–14%, improved member experiences, and growth to approximately 350,000 members as a product of that relationship—the two organizations announced in February 2021 that they had committed to a long-term agreement that extends the joint-venture relationship.17
It’s not a new concept
While many health systems view the payvider solution as a daring new model, the reality is that this concept has been around in the healthcare environment for nearly a century. Although the term “payvider” was still decades away, the model was introduced in the 1920s.18 With the onset of the Great Depression, providers initiated the original form of health insurance, offering care services to individuals on a prepaid basis.19 It was the first employer-sponsored hospitalization plan and the forerunner of the modern HMO, a strong idea that led to the creation of Blue Cross organizations.20
How and where to start a payvider solution
According to Contigo Health, the best place for a health system to begin its payvider solution is right at home with its own employee health plan. There they can learn and grow in a more controlled and familiar environment. Then, leveraging the knowledge, experience, and credibility gained through their own program, they can expand with the engagement of local self-insured employers who would benefit from the health system’s payvider solution. Methodically, the payvider solution can then be sold to larger employers, including those having multiple locations in multiple markets.
The need is clear, and the time is now
By all indications, with health systems facing relentless pressures and a more imminent need for change—combined with favorable forces of evolving technology, regulations, and market dynamics—the time of the payvider movement has arrived. In the remainder of this three-part series, we will present additional insight to help health systems take advantage of this unique opportunity.
© 2023. CONTIGO HEALTH, LLC. ALL RIGHTS RESERVED.
Sources
1. Fierce Healthcare. 2018. “More providers enter joint ventures with insurers to create health plans.” February 2018. Link. Accessed August 31, 2023.
2. West Monroe. 2022. “2023 Outlook: The Future of the Healthcare Industry.” December 2022. Link. Accessed August 30, 2023.
3. Change Healthcare. 2018. Report: “Finding the Value: The State of Value-Based-Care in 2018.” June 2018. Link. Accessed August 30, 2023.
4. Paul Keckley. The Keckley Report. July 11, 2022. Link. Accessed August 30, 2023.
5. U.S. Bureau of Labor Statistics. 2022. “Employment Projections: Median Age of the Labor Force, by Sex, Race, and Ethnicity.” September 2022. Link. Accessed August 31, 2023.
6. National Library of Medicine. 2021. “Metabolic Syndrome Incidence in an Aging Workforce: Occupational Differences and the Role of Health Behaviors.” July 28, 2021. Link. Accessed August 31, 2023.
7. City of Hope. 2023. “Why Are Cancer Rates Rising in Adults Under 50?” January 2023. Link. Accessed August 31, 2023.
8. EBRI. 2022. “Use of Health Care Services for Mental Health Disorders and Spending Trends.” September 2022. Link. Accessed August 31, 2023.
9. Healthcare Finance. 2016. “25 Biggest Provider-Sponsored Health Plans Include Some of the Nation’s Biggest Health Systems.” September 2016. Link. Accessed August 31, 2023.
10. Kaiser Permanente. 2023. Kaiser Foundation Health Plan and Hospitals Q2 2023 Financials. August 4, 2023. Link. Accessed August 30, 2023.
11. Cision PR Newswire. 2023. Kaiser Foundation Health Plan and Hospitals Report 2022 Financial Results. February 10, 2023. Link. Accessed August 30, 2023.
12. eHealth. 2022. Best Health Insurance Companies Compared. October 28, 2022. Link. Accessed August 30, 2023.
13. Forbes. 2023. Kaiser Permanente Health Insurance Review 2023. January 3, 2023. Link. Accessed August 30, 2023.
14. Value Penguin/Lending Tree. 2023. Kaiser Permanente Insurance Review: Why Is It Top-Rated? July 25, 2023. Link. Accessed August 30, 2023.
15. Frontiers of Health Services Management. For UW Health, Health Plan Ownership Provides Financial Stability. Kaplan, Alan S. FACHE. Summer 2023. Link. Accessed August 30, 2023.
16. Beckers Hospital Review. 2021. It’s Time for Payvider Adoption and Growth. June 16, 2021. Link. Accessed August 30, 2023.
17. Ibid.
18. Wikipedia. Health Insurance in the United States, History. Link. Accessed August 30, 2023.
19. Ibid.
20. Ibid.
© 2024. Contigo Health, LLC. All rights reserved.
Publication: Employee Benefit News
September 28, 2023
Whenever your employees need out-of-network care, they may be faced with unanticipated costs that can be eased with the right network solutions. By reconsidering various offerings and making the right choices, your organization can save money — while making their healthcare costs more predictable.
Gain complimentary insights into:
- The evolving landscape of out-of-network care
- How to maximize savings by understanding the lifecycle of a claim
- How employers can access multiple cost containment solutions without obligation
Source URL: https://www.benefitnews.com/web-seminars/the-murky-waters-of-out-of-network-claims
*Courtesy of Employee Benefit News
© 2024. Contigo Health, LLC. All rights reserved.
Premier, Inc.
June 21, 2023
Key takeaways:
- The Premier Trailblazer Award – Life Science and the Premier Trailblazer Award – Employer will be given for the first time this week during Premier’s Breakthroughs Conference and Exhibition.
- These awards recognize achievements in the use/deployment of innovative and scalable methods and technology to accelerate clinical evidence into real-world practice.
- Congratulations to AstraZeneca and Walmart, recipients of this year’s Trailblazer Awards!
Premier’s annual Breakthroughs Conference and Exhibition is in full swing in Nashville, Tennessee, this week and part of the excitement is the presentation of awards and special recognitions to our members, suppliers and others that have stepped up their game in transforming healthcare in the communities they serve throughout the year. These include our Innovation Celebration, Alliance Excellence Award, Cares Award, various member and supplier performance awards, and new this year – the Trailblazer Awards.
We are thrilled to celebrate the achievements of AstraZeneca, winner of the first Trailblazer Award – Life Science and Walmart, winner of the first Trailblazer Award – Employer!
AstraZeneca is a science-led, patient-centered company that develops innovative medicines for millions of people globally. The company leads a diverse area of therapy focus for oncology, biopharmaceuticals and rare disease that includes cardiovascular, renal and metabolism (CVRM), respiratory and immunology (R&I) and vaccine and immune therapies (V&I).
AstraZeneca and Premier’s PINC AI™ Applied Sciences (PAS) team have partnered over the past 15 years to design more than 37 projects involving clinical trials, prospective and retrospective research, feasibility studies and data and evidence generation. These projects focus on bridging the gap between life science innovations and implementation in various therapeutic areas.
Our collaborative work in oncology care was formally recognized in September 2022 with a Biotech Week Boston (BWB) Award in Digital Medicine for bold and innovative creation or use of technology-enabled healthcare solutions that are propelling technology forward and solving a healthcare need.
Walmart: Trailblazer in Employee Health Plan Innovation
Walmart is an iconic retailer and employer of 2.1 million people across 10,500 business units in 20 countries. In the U.S., more than 1.6 million associates rely on Walmart’s comprehensive suite of benefits that gives them and their families access to affordable, quality care to support all aspects of life – when, where and how they need it. Walmart’s progressive health benefits include its high-performing centers of excellence (COE) programs under the leadership of Walmart’s Lisa Woods, Vice President, Physical and Emotional Wellbeing, and her team.
Walmart and Premier’s Contigo Health have partnered over the last decade to design evidenced-based, market-leading COE programs focusing on Spine, Joint, Cardiac and Bariatric Surgery. The patient-centered specialty programs include extensive provider vetting, direct-to-provider contracting, collaborative care decision-making focused on quality and appropriate care, bundled payments, concierge patient experience, and lower costs with better outcomes.
In a Harvard Business Review article, Contigo Health’s Chief Medical Officer Jonathan Slotkin and Walmart’s Lisa Woods shared that half of spine patients avoided surgery, and spine surgery patients returned to work 20 percent sooner than their non-COE counterparts.
Congratulations to our first Premier Trailblazer Award winners!
AstraZeneca will be recognized during this evening’s Breakthroughs keynote session and Walmart will be recognized during tomorrow morning’s thought leadership session. All conference attendees are welcome to join us in celebrating their trailblazing achievements.
© 2024. Contigo Health, LLC. All rights reserved.
By:
Steven Nelson
President, Contigo Health
Britt Hayes
Chief Commercial Officer, Contigo Health
The healthcare industry itself is not immune to the challenges of managing health benefits costs for its own workers. Benefit administrators for health systems are faced with the same challenge that all employers are addressing in 2023 and beyond: how to provide employees with the highest-quality care while optimizing costs and maximizing plan flexibility for both their healthcare employees and the organization. For U.S. companies, the cost of caring for more than one in two Americans receiving insurance through employer-sponsored plans continues to increase.¹
For larger employers, the total cost of health benefits further rose by 5.3% in 2021.² Even as they provide care to others, many health systems’ associates are seeing increases in their insurance premiums that are outpacing inflation and wage growth. In fact, the average annual health insurance premiums for family coverage for employer-sponsored health plans have topped $20,000 for the first time, according to KFF 2018. On average, covered workers contribute 18% of the premium for single coverage and 30% of the premium for family coverage. Total costs for these premiums increased by 22% from 2014 to 2019, and worker contributions increased by 25% during that time.³ To better manage the cost of care, employers across all sectors have transitioned to self-funding options. Today more than 61% of some 150 million people receiving employer-sponsored insurance (ESI) are covered by self-funded or partially self-funded healthcare plans.
In very large companies with 5,000 or more employees, 91% of workers are in self-funded plans, and the rate of adoption among smaller organizations continues to accelerate.⁴ Just like any other self-funded employer, health systems generally require some type of third-party administration (TPA) solution to administer their health plans. Some use carriers or health insurance companies that market “administrative services only” (ASO) options for their TPA functions. Others use traditional TPAs. A partnership with a specialty TPA that offers deep expertise in the intricacies of managing health benefits for healthcare workers, however, has the potential to be transformative across a health system’s entire organization.
For larger employers, the total cost of health benefits in 2021 is expected to further rise by 5.3%.
For the first time, average annual health insurance for employer-sponsored health plans have topped $20,000 per family.
Plan Management In a Complex Environment
Health systems must consider a myriad of business factors when evaluating a TPA relationship. In addition to the increasing costs of employee care, they are immersed in a volatile industry environment of skyrocketing patient care costs, tight operating margins, reimbursement pressures, complex partner relationships, and moves to new care-delivery models that require greater transparency. At the same time, they are also struggling to balance the benefits of new technologies with EMR and data management complexities, ever-changing regulatory issues, aging patient populations with more complex medical issues, and highly competitive workforce challenges. Adding to the current landscape is the impact of COVID-19.
Coupled with so many other issues, the pandemic has put even greater stress and uncertainty on the country’s healthcare system. These complications can make the prospect of transitioning to a TPA plan or a new TPA partner seem overwhelming for a health system. Yet the urgency to deliver quality care at lower costs, without compromising service and positive member experiences, is greater than ever before. Forging a relationship with the right TPA that has extensive expertise and flexibility can be an ideal solution for many health systems, despite the perceived complexities of making such a move. This is particularly true for larger health systems that have already invested heavily in quality health solutions for their employee population. They require a highly flexible plan that optimizes these investments, with options that fit specific needs of employees.
Specialty TPA Advantages for Differing Priorities
Simply put, self-funded organizations may choose a specialty TPA with deep health systems expertise to gain more control over their destiny than they could achieve in a traditional carrier relationship. That greater control can translate into flexible options in benefit design, data integration, population health tools (leveraging CINs and ACOs), and nondomestic network coverage, as well as substantial business reimbursement for patient care. It can also mean more significant opportunities to utilize their clinical strengths in caring for the organization’s employees. A specialized TPA relationship can address this need for control and customization, and it can respond to differing priorities across the system. From HR to finance to clinicians and business development, each function can realize positive impacts from an effective TPA partnership. Working with a TPA that is attuned to a health system’s entire ecosystem helps to create a personalized approach that empowers unprecedented collaboration.
A Tailored Approach
For the HR team at a health system, the TPA partner must be an expert in designing flexible plans targeted to the current and changing needs of the system’s workforce. It should have the capabilities to introduce new and innovative options for the health system’s most discerning population: its associates. The plan design must also integrate seamlessly with existing health management programs, such as PBMs, ACOs, and clinically integrated networks (CINs). The working relationship with the TPA partner is also a significant factor in helping to ensure the success of the plan. HR benefits administrators should expect high levels of service, responsiveness, objectivity, and useful reporting tools from the TPA.
Forging a relationship with the right TPA that has extensive expertise and flexibility can be an ideal solution for many health systems.
Working with a TPA that is attuned to a health system’s entire ecosystem helps to create a personalized approach that empowers unprecedented collaboration.
Domestic Utilization and Cost Management
For CFOs charged with cost and risk management across all aspects of the organization, a strong TPA relationship will help facilitate cost-containment opportunities. By focusing on actual costs rather than carrier rates, a well-designed plan can provide direct savings that remain within the health system. A TPA that possesses health system insights and expertise can identify opportunities for maximizing domestic utilization rates, which can contribute significantly to overall system revenue generation and employee benefits cost control. An experienced, employee-focused TPA will be able to lead a thorough analysis to assess gaps in quality of care and provider networks to strengthen domestic utilization. When health systems employees and their health plan dependents use the actual services they provide, they help contribute to building a stronger community and stronger brand while taking advantage of the quality of care provided by the health system.
Network providers can realize more financial benefits, and systems can play an active role in improving their staff’s health outcomes. By directly assessing and managing claims data while maintaining patient confidentiality or PHI integrity, health systems can find ways to mitigate rate increases over time. Utilization is vitally important in today’s healthcare environment. Increases in domestic utilization can make a difference when it comes to containing spiraling costs. From 2016 to 2017, spending rose 4.2%, while prices jumped 3.6%, but healthcare utilization only grew by 0.5% during that time, illustrating dramatic opportunities for improvement.⁵
Data-Driven, Patient-Centered Care
As CMOs, CQOs, and CIOs work with their systems to focus on strategies that deliver quality, data-driven, patient-centered care more effectively, a customized plan can make meaningful contributions toward these efforts. In an ideal scenario, health systems want to further improve their population health through a TPA relationship that can include tools to help tap real-time clinical information, enabling them to achieve optimal levels of appropriate care. Virtually every health system has invested heavily in data, technology, and EMR as mission-critical assets. U.S. health IT spending topped $7.1 billion in 2017 and continues to increase annually.⁶ Partnering with a TPA that has access to clinical data decision-support tools can help providers deliver a tailored plan to allow providers to offer the right care, at the right time, in the right setting, at the right costs. Leveraging these tools can help address targeted variations, thus enabling flatter overall medical trends.
A TPA with health system insights and expertise can identify opportunities for maximizing domestic utilization rates, which can contribute significantly to overall system revenue.
U.S. health IT spending topped $7.1 billion in 2017 and continues to increase annually.
Recruitment
A personalized plan can also serve as a powerful recruitment tool. HR teams must attract talent with a robust, affordable, and flexible health benefits package that enhances members’ experiences. Many employers are recognizing this need. The number of those who view their healthcare offerings as an integral part of their workforce strategy increased from 36% in 2019 to 45% in 2020.⁷ The right plan that includes work-life balance/flexibility programs, support for innovation, and mentoring opportunities can also be an essential retention tool for health systems employers in a highly competitive job market.⁸ According to a recent survey, more employees in the healthcare sector report they have been actively looking for a job during the past year than in other sectors.⁹
Business Development
Business development teams are seeking new revenue-generation opportunities. For some health systems, an optimized self-funded plan can help create direct relationships with non–health system employers looking for a better way to achieve their health benefit goals. The plan can serve as a model and a facilitator for initiating new relationships with employers in order to pursue broader strategic aims and increase market share.
Overcoming Barriers
A self-funded plan with a specialty TPA relationship can be a tremendous advantage for the right health system. But it is not always a solution for every organization. All potential barriers and objections should be assessed, along with timing, before considering a shift. For instance, the arrangement requires knowledgeable benefit administration skill sets to make the most of the TPA relationship. If the level of internal expertise is not currently present, the organization may need to invest in staffing to build or train the right teams. The same is valid for health systems that may be considering self-funding their health benefits plan as a precursor to delivering direct-to-employer offerings. Other barriers may include organizational concerns about disrupting long-standing relationships with current payors or moving from a large partner with a known brand to a nimble and specialized but lesser-known entity. In addition, an organization’s leadership may not recognize the potential value of a specialized TPA relationship without a thorough analysis of the positive impact it can have on the entire organization. HR teams should align with finance teams and be prepared to make the case. Changing the status quo in any organization is an educational process, and the transition to a new or different TPA relationship will require a thoughtful strategy. The goal should be to engage all stakeholders and address possible concerns while conveying the cost and operational benefits that can be realized. A specialty TPA partner with the requisite depth and breadth of health system experience can assist in helping to remove these barriers.
A personalized plan can also serve as a powerful recruitment tool.
For some health systems, an optimized self-funded plan can help create direct relationships with non-health system employers looking for a better way to achieve their health benefit goals.
HR teams should align with finance teams and be prepared to make the case.
Contigo Health: Uncomplicating the Complicated
Today’s healthcare world is more complex than ever before. Building a self-funded plan requires a TPA partner that will help “uncomplicate the complicated” while facilitating quality care, cost savings, and innovation. An experienced TPA partner understands the unique complexities of health systems and can effectively navigate self-funding design and implementation to realize the plan’s full potential across the entire organization. While numerous TPAs exist, health system decision-makers must closely examine the additional value a specialty TPA can offer. Contigo Health® Sync Health Plan TPA is redefining health systems’ expectations for TPA services with an exciting combination of offerings and continuous innovation. In addition to its legacy of TPA leadership, Contigo Health, formerly Health Design Plus (HDP), is backed by the strength and resources of its affiliation with Premier, Inc, a leader in data, analytics, consulting, and group purchasing for health systems.
Partnership Benefits
- Contigo Health offers leading-edge, TPA custom solutions designed expressly for health systems
- A client roster featuring leading employers known for quality and innovation in health benefits delivery
- Strategic analysis, design, and integration with existing health management programs
- Flexible, objective benefit design for greater control in payment models, data integration, and network coverage
- Comprehensive reporting tools and protection of confidential information
- Exceptional client relationships, with a proven track record reflected by exceptional client retention and consistently high Net Promoter scores
- Experienced, responsive, and friendly service from a professional, caring, and hardworking team that delivers unparalleled support
-
Close examination of the additional value
-
Combination of offerings and continuous innovation
-
Legacy and leadership backed by strength and resources
Not already self-funded? For health systems that are not already self-funded, Contigo Health can lead the transition when they are ready to make the change.
Ready to learn more? Speak with a Contigo Health Representative today at 330-656-1072 or visit contigohealth.com.
1. Berchick, Edward R., Hood, Emily, and Barnett, Jessica. 2018. “Health Insurance Coverage in the United States: 2017.” United States Census Bureau. September 12, 2018. https://www.census.gov/library/publications/2018/demo/p60-264.html
2. Business Group on Health. 2020. “2021 Large Employers’ Health Care Strategy and Plan Design Survey.” August 2020. https://www.businessgrouphealth.org/resources/2021-large-employers-health-care-strategy-and-plan-design-survey
3. Kaiser Family Foundation (KFF). 2019. “2019 Employer Health Benefits Survey.” September 25, 2019. https://www.kff.org/health-costs/report/2019-employer-health-benefits-survey/
4. KFF Survey. 2019. https://www.kff.org/health-costs/report/2019-employer-health-benefits-survey/
5. Health Care Cost Institute (HCCI). 2019. “2017 Health Care Cost and Utilization Report.” February 11, 2019. https://healthcostinstitute.org/annual-reports/2017-health-care-cost-and-utilization-report
6. Spitzler, Julie. 2018. “Health IT spending last year prioritized EMRs.” Becker’s Health IT. January 29, 2018. https://www.beckershospitalreview.com/healthcare-information-technology/health-it-spending-last-year-prioritized-emrs.html
7. Business Group on Health Survey. 2020 https://www.businessgrouphealth.org/resources/2021-large-employers-health-care-strategy-and-plan-design-survey
8. America’s Health Insurance Plan. 2018. “The Value of Employer-Provided Coverage.” February 2018. https://www.ahip.org/wp-content/uploads/2018/02/AHIP_LGP_ValueOfESIResearch_Print_2.5.18.pdf
9. Deloitte Development LLC. 2013, “Talent 2020: Surveying the talent paradox from the employee perspective – The view from the Health Care sector.” September 2012. https://www2.deloitte.com/us/en/pages/human-capital/articles/talent-2020-paradox-health-care-sector.html
Disclaimer: Forward-looking statements are predictive in nature and reflect the authors’ beliefs at the time of the statement. Embedded links are accurate at the time of publication and are subject to change. Reasonable efforts have been made to ensure that the information contained herein is accurate and from reliable sources. Contigo Health, LLC, is not responsible for any errors or omissions, or for the results obtained from the use of this information.
© 2024. Contigo Health, LLC. All rights reserved.
InsideOut Podcast
June 15, 2023
On this episode of InsideOut, Michael Alkire, Premier, Inc. President and CEO, welcomes co-host Dr. Jonathan Slotkin, Contigo Health’s Chief Medical Officer and guest, Lisa Woods, Vice President, Physical and Emotional Wellbeing of Walmart to discuss their strong commitment to healthcare and the comprehensive and cost-effective benefits in place for their employees.
Source URL: https://premierinc.libsyn.com/walmart-on-the-employers-role-in-healthcare-transformation
© 2024. Contigo Health, LLC. All rights reserved.
A new purpose-built national wrap network could minimize cost, simplify the claims process, and make out-of-network care less painful for employer-funded health plans.
The need to strike a balance between provider access and cost of care is perhaps most profound in an employer’s wrap network.
Introduction
According to a national survey, employers recognize that their health benefits plans are playing a more pronounced role in attracting and retaining employees, especially since the pandemic. Two-thirds of employers consider health benefits as vitally important in their management of talent. But while employers are seeking to expand their health benefits offerings—a broader provider network being one of the most important factors—they are highly concerned about managing the cost of care. The latter point is particularly significant as most employers (60%) have seen their healthcare costs outpace inflation over the past three years and expect that trend to continue.¹
While many health plan provider networks are comprehensive, plan members still venture beyond the reach of their primary network. Whether they are traveling or close to home, employees and their dependents sometimes choose to engage providers that are not within their plan’s established network. That’s when a wrap network comes in.
Wrap networks are designed to enable access to care when plan members do opt to seek care from a specialist that is not in the health plan’s primary network. The challenge for employers is that with little or no provider fee boundaries nor sufficient pricing transparency, out-of-network care is often financially distressing to health plans and the employees and families they serve. While employers are willing to give their health plan members the choice to seek care out of network, there is also a need to establish greater cost control for that care. Unfortunately, HR decision makers tend to have little familiarity with and understanding of wrap networks.
The employers who are familiar tend to be satisfied with the breadth and quality of their wrap network but are often extremely dissatisfied with the associated expenditure. These employers consider the most important attributes of a viable wrap network solution to be controlling the cost of access to providers, pricing transparency, and cost savings greater than currently available options.
“The intent is to be able to bring more transparent network products to the market—especially in areas where transparency has been lacking, such as with out-of-network care. We are rethinking out-of-network wrap products to align them with what employers tell us they value most—cost savings and transparent pricing.”
Robin Bugni,
Contigo Health’s VP of Network Product & Development
Considering the lack of awareness and understanding of wrap networks and the level of dissatisfaction with the cost of out-of-network care, there is a significant opportunity for a better wrap network solution, one that delivers valued network breadth while also directly lowering medical claims costs through defined discounts and pricing transparency—in other words, building a wrap network that delivers on what matters most to employer-funded health plans. There is substantial employer interest in ConfigureNet™, a compelling wrap network model from Contigo Health® intended to address the access-versus-cost challenge by extending comprehensive coverage in all 50 U.S. states and across specialties while simultaneously introducing a level of cost savings through pre-negotiated provider pricing and a streamlined process that is direct to employers.
The high cost of out-of-network care
Out-of-network care has traditionally been more costly to a health plan and its members than in-network care. Out-of-network providers have had the freedom to charge higher rates since they are not bound by the health plan’s contracted primary provider network reimbursement. Out-of-network providers have no obligation to accept the reimbursement amount the health plan is willing to pay its in-network providers. This commonly leads to the practice of balance billing, where the provider charges the patient an amount above what the health plan paid and up to the provider’s originally billed amount. This can be an unpleasant surprise to health plan members and the health plan itself.
Beyond the provider reimbursement difference, the medical claims repricing progression often involves multiple intermediaries providing various services for which each can take its own administrative fee, adding more unexpected administrative cost to the health plan.
Contigo Health, LLC, as an architect of financially sustainable healthcare, has taken steps to identify a key area where a more contemporary model with real cost controls and pricing transparency could help employers address the care and cost imbalance of out-of-network care.
A survey about wrap networks
To gain a better understanding of current perceptions about wrap networks, and to reveal what gaps and opportunities there may be to improve those networks, a study was conducted by Stonegate in April of 2022.²
The survey focused primarily on input from health system employers—specifically HR decision makers and health system executives. This audience represents leadership in healthcare delivery, intimate knowledge of healthcare infrastructure and pricing, and perspective as one of the largest employers in a market. The findings complement broader industry studies regarding employer perceptions of care versus cost. The results revealed four distinct areas of interest for anyone desiring to create a better wrap network solution for their health plan.
How familiar are you with the word “wrap network”?*
*Sample size is 25.
Familiar (familiar) – 60%
Very Unfamiliar (somewhat to very) – 28%
Very Familiar (somewhat to very) – 12%
Nearly half (46%) of HR decision makers indicated they are neutral to extremely dissatisfied with the cost of their wrap network access.
Four things that employers should know about wrap networks
1. Health plan decision makers don’t tend to understand wrap networks.
An interesting discovery from the Stonegate study is that employers, by and large, do not appear to have a strong awareness of wrap networks, let alone an understanding of the costs associated with such networks. Among the HR decision makers surveyed:
- Nearly 1 in 3 (28%) are very unfamiliar with the term “wrap network.”
- Most (57%) admitted they don’t understand the costs associated with their current wrap network. Just 43% said that they definitely understand the costs.
This gap in understanding is an opportunity for a new wrap network solution that can deliver needed clarity, consistency, simplicity, and support. For those that do have an understanding of their wrap networks, the study revealed some valuable insight into what matters most to them, as is revealed in the next sections.
2. Breadth and quality get high marks. Cost, not so much.
The Stonegate-conducted study asked employers to identify the best and worst attributes of their current wrap network. The survey revealed that health plan decision makers are largely satisfied with their current wrap networks when it comes to the breadth and quality of network access.
- 85% are extremely satisfied with the extent of their wrap network
- 85% are extremely satisfied with the quality of network access
HR decision makers identified the following as the most important wrap network access and quality attributes.
Importance of access and quality attributes to HR decision makers
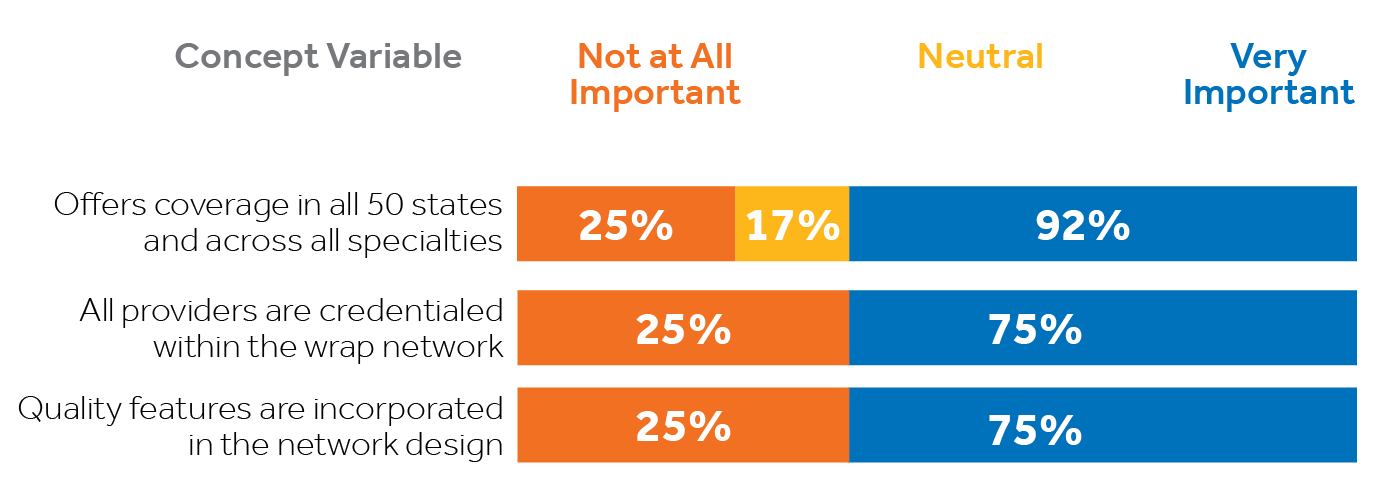
As encouraging as that is, employers are clearly less than satisfied and more concerned with the cost of that access. In fact, cost is the highest area of dissatisfaction among health system employers surveyed specific to wrap networks. Nearly half (46%) of HR decision makers indicated they are neutral to extremely dissatisfied with the cost of their wrap network access. That percentage may be conservative considering, in section 1, it was revealed that 57% of HR decision makers surveyed do not even understand the costs associated with their wrap networks.
3. It comes down to economics.
The aspects of a wrap network that rose to the top among health plan decision makers surveyed by Stonegate consistently involved three areas: cost containment, pricing transparency, and cost savings. These are the characteristics identified as VERY IMPORTANT to employers:
- 100% indicated cost-containment when accessing out-of-network providers
- 100% emphasized pricing transparency
- 92% want more savings than what’s currently available
- 92% want a configurable wrap solution that meets their specific needs
Importance of economic wrap network attributes to HR decision makers
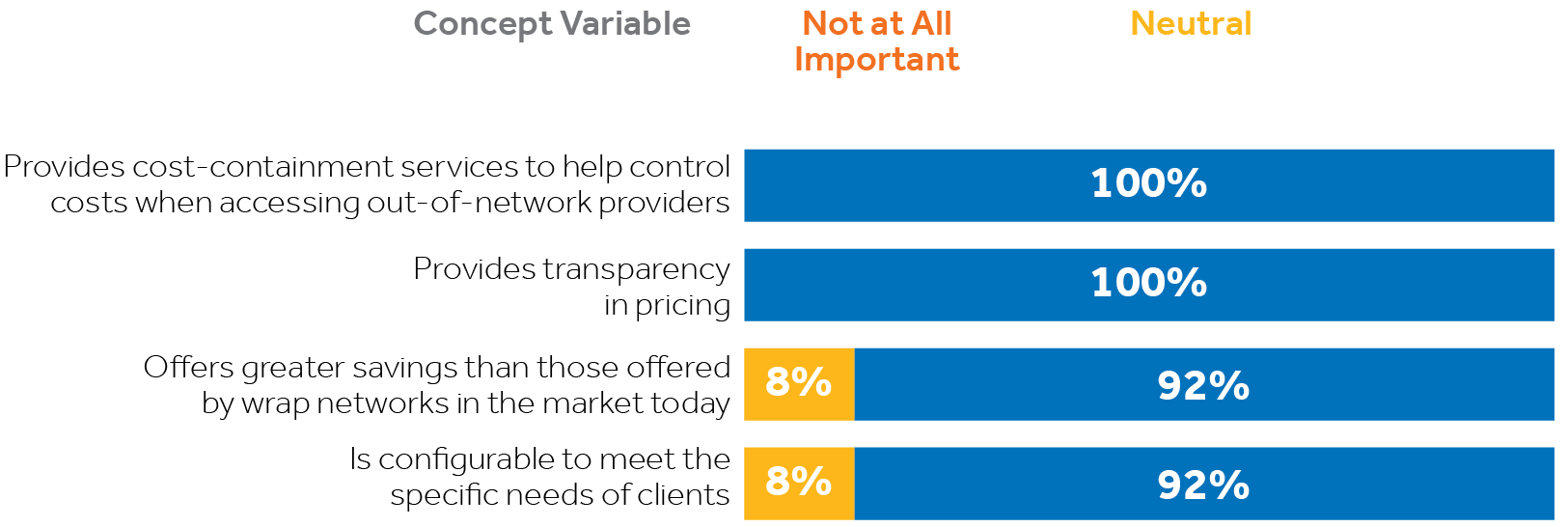
In consideration of the first three core study findings listed above, it is evident there is call for a more suitable wrap network solution for employers than is currently available. A better wrap network product would directly address employers’ cost concerns without compromising their plan’s access to care. The optimal solution would deliver on all the things that matter most to employers, including breadth and depth of their wrap network access, plus significant cost savings beyond the industry status quo, along with much-needed pricing transparency—in other words, securing the lowest possible price and eliminating unexpected charges without compromising access to care.
“Contigo Health’s charge is to be the architect of better, more sustainable healthcare. We are building the foundation for future network structures from the ground up by helping to reduce the cost of out-of-network care, should people need it.”
Steven Nelson, President,
Contigo Health
4. One solution is showing great promise.
There is significant interest among health system HR decision makers and executives in a new wrap network product pioneered by Contigo Health. Known as Contigo Health® ConfigureNet™, this contemporary wrap network product is structured to provide the coast-to-coast national coverage and key specialties that employers value highly. The wrap is differentiated in that it has been designed to introduce significantly discounted provider rates and a high level of pricing transparency, combining to enable a level of cost savings greater than what is currently available in the market. As the name suggests, ConfigureNet™ is also designed to eventually become configurable to meet the distinct needs of individual employers.
Developed specifically to meet the needs most emphasized by employers, ConfigureNet™ provides health plans with robust out-of-network provider access at a lower cost. The following features directly address those expressed needs:
Broad network coverage spanning all 50 U.S. states plus Puerto Rico
Pre-negotiated contracted discounts with 900,000 U.S. providers and 4.3 million U.S. locations
Better negotiated rates and greater savings
Contractual protection from surprise balance billing
Claims repriced promptly to contracted rate—no additional handling or unwarranted additional fees
ConfigureNet™ introduces nationwide access to contracted healthcare providers with pre-negotiated discounts in place for a full range of provider services including:

70% of executives and 67% of HR decision makers find the ConfigureNet™ wrap network concept very appealing.
A majority of Stonegate survey respondents find the ConfigureNet™ wrap network concept very appealing.
How executives view the ConfigureNet™ wrap network concept
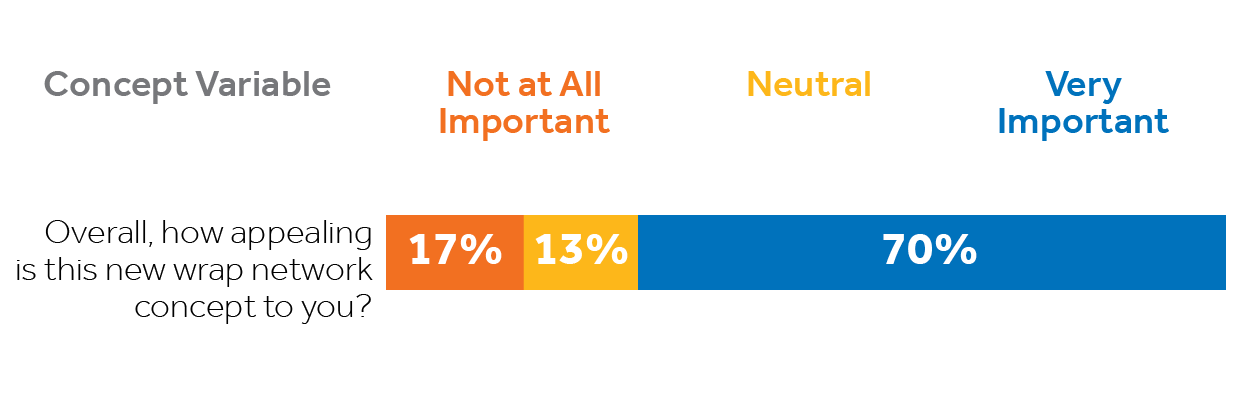
How HR decision makers view the ConfigureNet™ wrap network concept
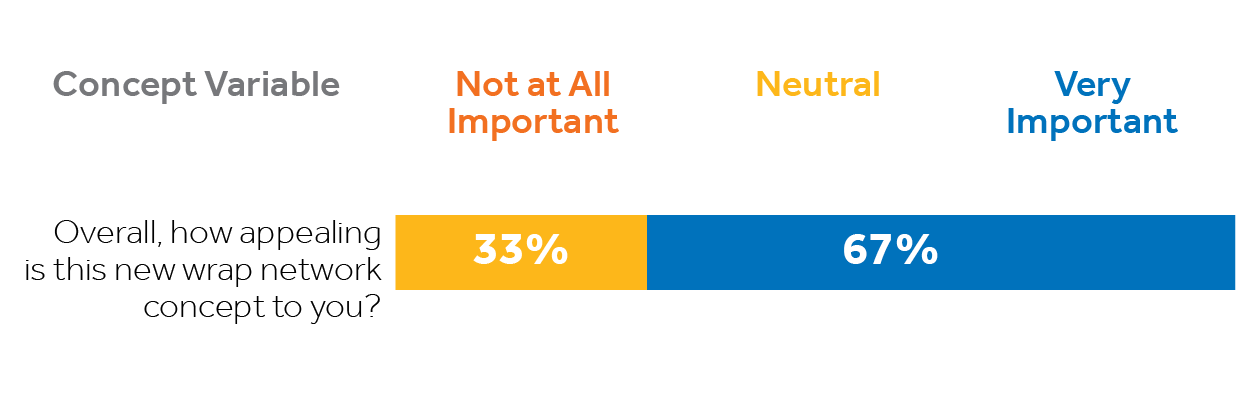
Contigo Health’s ConfigureNet™ out-of-network wrap solution has tremendous appeal because it addresses employers’ most pressing wrap network concerns while presenting features that matter most. Fifty percent of surveyed executives would definitely consider switching their wrap network if doing so would provide financial benefits to their organization. A third of HR decision makers and 30% of executives would consider carving out their wrap network from their current plan.
SUMMARY
Health benefits—including expanded out-of-network coverage—are increasingly important to employers as they place greater emphasis on attracting and retaining talent. Even so, they have serious concerns about managing the rising costs associated with those benefits, especially the high cost of out-of-network care.
Unfortunately, many employer-funded health plan decision makers and executives are either unaware of their wrap network or do not understand it. But compelling gaps in current wrap networks have been revealed in recent data, indicating there are attractive opportunities to provide employers with a better, more viable out-of-network solution that addresses the distinct attributes and performance characteristics decision makers have indicated are most important to them.
Employers who have a more thorough understanding of wrap networks appreciate the breadth of their current plans’ access to out-of-network care but, at the same time, are frustrated by the associated costs and lack of transparency. They would welcome a solution that substantially cuts their out-of-network costs without compromising valued access to care. Contigo Health’s new ConfigureNet™ wrap network appeals broadly because it is designed to give health plan decision makers more control of their wrap network. ConfigureNet™ preserves the merits of a broad and robust provider network (what employers like) while substantially controlling costs (what employers want). This is accomplished through contracts with 900,000 U.S. providers and more than four million locations coast-to-coast, and introduces pre-negotiated discounts, pricing transparency, and a streamlined process that can cut unwarranted additional fees. It can empower health plan administrators to impact their organization’s bottom lines while enhancing access and choice for their health plan members.
What solution will you bring to your health plan?
ConfigureNet™ has tremendous appeal to employers because it addresses their most significant wrap network concerns directly and delivers the attributes that matter most. Fifty percent of executives surveyed would “definitely consider switching” their wrap network if doing so would have financial benefits for their organization. That is why 37% of executives expressed they would be very interested in a no-cost consultation to compare the costs of ConfigureNet™ to their existing wrap network.
Leveraging its ConfigureNet™ nationwide provider network, Contigo Health has also created ConfigureNet™ Price Advantage, a flexible plug-in that gives employers a smart, “on-demand” repricing solution when and where it is needed most. It can be implemented as their dedicated
out-of-network cost-containment solution, or configured as a cost-saving option to expand the power of out-of-network cost containment solutions that may already be in place. Price Advantage was designed to be a no-risk, no obligation alternative.
See how Contigo Health can help you establish clear savings on your out-of-network wrap by conducting a complimentary out-of-network wrap cost analysis for each.
How it works:
1. You share health plan claims data
2. Contigo Health analyzes the health plan’s existing out-of-network claims data for the past year and identifies savings potential (two-week turnaround)
3. We meet to review and discuss savings opportunity and quote
4. Contigo Health creates a contract to make an easy and frictionless switch
For more information, contact Britt Hayes, Contigo Health’s Chief Commercial Officer at Britt.Hayes@contigohealth.com, or call 330-656-1072.
1. Aditya Gupta, Nikhil Mahajan, Carolina Malcher, Monica Qian, Matthew Scally, and Jeris Stueland, “Employers Look to Expand Health Benefits While Managing Medical Costs,” McKinsey & Company Employer Health Benefits Survey (May 25, 2022) source
2. ConfigureNetTM and Beckers, Health Plan Wrap Networks Perceptions survey (conducted by Stonegate), April 2022
© 2024. Contigo Health, LLC. All rights reserved.
